This is an active journal, initiated October 04, 2024. Follow along as I progress from Achilles injury to recovery. Updated periodically.
Introduction
One free throw, one moment, and suddenly my life changed with a ruptured Achilles. What started as a simple injury became a journey of surgery, recovery, and reflection. This diary isn’t just about healing; it’s about facing unexpected challenges, learning to embrace the suck, and finding resilience. Through these entries, I’ll share my path from surgery to recovery, the physical and emotional ups and downs, and the lessons that emerged along the way. 61-year old male. Jump to Timeline
Pain is personal and varies greatly. My post-surgery pain has fluctuated between 1 and 3 out of 10, which felt manageable. A 3/10 for me might feel like a higher level for someone else, or vice versa. We all have our own tolerances, so it’s essential to recognize that pain isn’t one-size-fits-all and to be compassionate toward ourselves and others in our pain journeys.
This is my story of healing – one step at a time.
 It was a crisp afternoon on 09/24/2024 at Camp Laurelwood in Madison, CT, where about 100 of us had gathered for our annual team-building event. The day was buzzing with energy, coworkers scattered around, participating in different activities. I found myself on an outdoor asphalt basketball court, attempting a free throw when it happened. Out of nowhere, it felt like someone had slammed into the back of my legs, hard. I went down immediately, tumbling and rolling a couple of times before I came to a stop. Confused, I turned around, still on the ground, and asked, “Who hit me?” The concern on my colleagues’ faces was clear, but they all shook their heads. “Nobody hit you, you just fell,” one of them said.
It was a crisp afternoon on 09/24/2024 at Camp Laurelwood in Madison, CT, where about 100 of us had gathered for our annual team-building event. The day was buzzing with energy, coworkers scattered around, participating in different activities. I found myself on an outdoor asphalt basketball court, attempting a free throw when it happened. Out of nowhere, it felt like someone had slammed into the back of my legs, hard. I went down immediately, tumbling and rolling a couple of times before I came to a stop. Confused, I turned around, still on the ground, and asked, “Who hit me?” The concern on my colleagues’ faces was clear, but they all shook their heads. “Nobody hit you, you just fell,” one of them said.
That’s when I knew something was seriously wrong. I couldn’t get up, and pain shot through my leg like a lightning bolt. With the help of a few colleagues, I managed to stand while they supported me, though my right knee was swelling from the impact of the fall. But it was my left foot that was the real problem, it felt completely useless. I couldn’t bear weight on it at all. Pain level was about 3/10 but the sense of dread was much worse.
Amy, my long-time good friend, drove me to the nearest emergency room, where they performed an ultrasound and X-ray. The confirmation hit hard: I had ruptured my Achilles tendon. I’d heard about Achilles injuries before, mostly in pro athletes, but nothing could have prepared me for what it meant to experience it firsthand. As I processed the news, I couldn’t help but think how quickly things can change. One minute I was shooting hoops with coworkers, the next, I was staring down months of recovery. Later that evening, equipped with new crutches, my wife Niki picked me up from the E.R. We drove home in silence, the weight of the day hanging heavy between us. There was so much unsaid, but I think we both felt it, this was going to be a long road.
By mid-morning on 09/25, I was sitting in the exam room at Connecticut Orthopedics, across from Dr. Spak. He carefully cut through the bandaging applied by the E.R. team and inspected my left calf. His expression told me what I had already suspected, it was a complete rupture of my Achilles. We talked through the options, weighing the pros and cons of surgery versus a non-surgical approach. In the end, we both agreed that surgery was the best path forward. It felt surreal hearing him lay out what was ahead, as if this injury had suddenly reshaped my entire immediate future.
We scheduled the surgery for Tuesday, 10/01, and that date felt like it became the focal point of everything in my mind. It was like my life was now split in two: before the rupture and everything that would come after. Before I left, his team fitted me with a large black Velcro walking boot. They even joked that it was the first time they’d had to issue a size XL boot. I also mentioned the fall I’d taken on my right knee, but since the swelling had already gone down, Dr. Spak reassured me it wasn’t anything to be concerned about.
Pain level was 1/10, but the emotional weight of it all was starting to settle in. The truth of what lay ahead was sinking deeper by the minute, and for the first time, I really started to grasp the road I was about to walk, figuratively, of course.
09/26 – 09/30
Two days after my Achilles injury, I began incorporating a series of stretches to maintain flexibility and prevent stiffness in my back and body. I committed to doing them two to three times a day, focusing on both seated and standing stretches, despite the challenges of balancing with my injured foot. These sessions helped keep me mobile and gave me a sense of control during recovery.
The days leading up to surgery passed in a blur. I was fortunate to spend this time relatively pain-free, encased in a boot that allowed me to bear some weight, even walk without crutches on good days. There was an odd mix of gratitude and frustration. Gratitude that the pain wasn’t worse, but frustration that I couldn’t do the things I was used to doing. I felt strong, but utterly limited. It was a lesson in patience I didn’t ask for.
Pre-op appointments came and went. EKGs, blood work, while balancing the logistics that came with a work-related injury. Workers’ compensation added another layer of complexity, with constant conversations with Deanna, my assigned nurse, filling the gaps between paperwork, forms, and work-from-home tasks. On top of that, my back had been acting up from the fall, making simple things like getting up from a chair a challenge. There were days where the back pain was more aggravating than my Achilles. Just when I thought I couldn’t juggle more, I was also processing three kidney stones. It’s like my body decided it was time for a complete overhaul all at once. Pain level still around 1/10, but I was definitely feeling worn out.
10/01 Surgery Day
The day arrived, and Niki and I made our way to the surgery center early, arriving at 06:00. The morning was quiet. After a brief wait, I was led to a prep room where I signed consents, got into a hospital gown, and had an IV started. I met Larry, the anesthesiologist, who discussed a nerve block for my left foot. “Let’s do it,” I said, resigning myself to whatever was necessary. After my lower leg was shaved, I was wheeled into the operating room. The room was cold, clinical, but I tried to keep things light, making a few jokes to ease my nerves.
When I woke up in recovery a couple of hours later, I felt surprisingly good. No pain, just a bit of grogginess and the odd sensation of my left foot being completely numb. The nerve block had done its job. Pain level was 0/10. I had trouble seeing out of my left eye oddly. I couldn’t understand why that was. There was also some soreness in my throat from being intubated, a normal process, though uncomfortable. Niki was by my side soon after, her presence a relief. Then, Larry stopped by. I mentioned the irritation with my left eye. He apologizes sheepishly for accidentally scratching my cornea during the surgery while positioning my face on the foam pad. It was just one more thing to add to the list, but at least it would heal soon.
We made our way home, and I kept reminding myself, this was just the beginning. Time to embrace the suck, as we say.
Coming home felt strangely surreal. The front steps, once so routine, were now my first real hurdle, forcing me into a deliberate, careful choreography with my crutches. No weight on my left foot, not even the tiniest misstep allowed. I was really appreciating the Crutch Underarm Pad Covers I ordered from Amazon to add padding and Marine flair to my crutches. The nerve block had fully taken over, my foot felt like it didn’t belong to me anymore. I couldn’t move my toes or feel the slightest twitch. The experience of a nerve block can feel both liberating and unsettling, providing pain relief but also robbing you of any sense of control over your body.
 The rest of the evening blurred by. Not so much in pain, but in a haze of fatigue and the constant sense of discomfort. Pain level 1/10. I had some chats with Deanna, keeping her informed of my status. My routine revolved around rotating from the couch to the deck, then to the chair in front of the TV, always with my foot elevated.
The rest of the evening blurred by. Not so much in pain, but in a haze of fatigue and the constant sense of discomfort. Pain level 1/10. I had some chats with Deanna, keeping her informed of my status. My routine revolved around rotating from the couch to the deck, then to the chair in front of the TV, always with my foot elevated.
The strangest part was setting up camp in Jake’s room. We lost our son Jake in 2020 to fentanyl poisoning, and since then, his room had felt like sacred ground, off-limits in a way. But now, with recovery requiring me to stay on the first floor, I found myself in there, and oddly, it felt comforting. Like he was watching over me in a way I hadn’t expected. Niki added a huge pillow under the foot of the mattress to keep my leg propped up. That little adjustment made a world of difference.
10/02 Post-Op Day 1
Waking up, the nerve block was still in full force, no feeling in my foot, but I’d slept well, with my leg propped up. My back was feeling better too, thanks to a foam mattress topper Niki added to the bed. The bathroom was still a bit of a mission, but I’ve gotten my system down. One crutch in hand, dragging a wooden chair alongside for balance, a makeshift second crutch. A small victory.
By 10:00, I started to feel the nerve block wear off, just a slight sensation returning to my foot. I could wiggle my toes, which was both a relief and a reminder of the pain to come. When Alyssa from the surgery center called to check in, we discussed my plan for managing the pain as the block wore off. I decided against Percocet and opted for Tylenol and Advil.
The rest of the day was about waiting. The nerve block wore down gradually, but the pain never really spiked. I stayed on top of the Tylenol and Advil, and it was enough to keep things manageable. I was lucky. By 22:30, the block was 50% gone, but I was handling it well. Pain level remained low, around 1/10.
10/03 Post-Op Day 2
Today’s my first post-op appointment with Dr. Spak, so I’m curious to see what his assessment is and what my next steps will be. I slept decently last night, which was a relief. I managed to get out of bed at 07:30 and my pain is at about a 2/10, which feels manageable. I took two Tylenol just to stay ahead of any discomfort. Now it’s time for some coffee to kick off the day and get my head straight before the appointment.
 11:00 First post-op appointment with Dr. Spak, and Niki was right there with me for support. Deanna also joined us. After a brief discussion about how I was feeling, Dr. Spak shared some encouraging news. He mentioned that next Thursday, he would be removing my stitches and fitting me for a boot, marking a significant step in my recovery. At that point, I’ll be introduced to minimal weight-bearing on my left foot, which feels like a big milestone. Dr. Spak was thorough in answering all my questions, and we agreed to revisit the topic of my return to work during my next appointment in a week. Overall, I left feeling optimistic about the progress I’m making in just a few days. Nerve block 100% gone. Took several days to subside. Foot still numb and pain level remains around 2/10.
11:00 First post-op appointment with Dr. Spak, and Niki was right there with me for support. Deanna also joined us. After a brief discussion about how I was feeling, Dr. Spak shared some encouraging news. He mentioned that next Thursday, he would be removing my stitches and fitting me for a boot, marking a significant step in my recovery. At that point, I’ll be introduced to minimal weight-bearing on my left foot, which feels like a big milestone. Dr. Spak was thorough in answering all my questions, and we agreed to revisit the topic of my return to work during my next appointment in a week. Overall, I left feeling optimistic about the progress I’m making in just a few days. Nerve block 100% gone. Took several days to subside. Foot still numb and pain level remains around 2/10.
10/04 Post-Op Day 3
Slept well last night, and I’m really appreciating the way we’ve set up the foot of the twin mattress to keep my leg elevated. It’s been a total game changer, making sure my foot stays propped up throughout the night. Took a couple of Tylenol around 02:30, and they did the trick. I’m still using the wooden chair as a second crutch to get to the bathroom. Dragging it in there and positioning it next to the toilet so I can rest my bad knee on it has been a lifesaver. Honestly, it makes those middle-of-the-night trips way easier, even on one leg! Morning pain level was steady around 2/10.
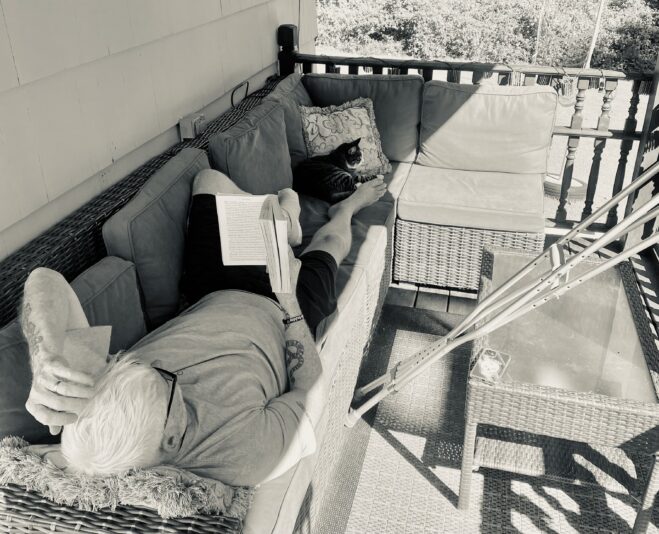
The day was mostly spent out on the back deck, enjoying the beautiful weather and reading. I stuck with my stretch routine and added in some creative push-ups against the kitchen island, trying to keep some level of fitness going. Ended the day with family, leg elevated, having dinner and a movie. Keeping spirits high. Right now, the main focus is keeping that foot elevated as much as possible and just embracing the process.
10/05 Post-Op Day 4
Another decent night—actually slept fairly well, all things considered. Woke up around 07:30 with that familiar dull ache, but nothing too intense. Reached for a couple of Advil to keep things manageable. Pain still holding steady at a 1/10, barely noticeable but just enough to remind me the journey’s still ongoing. Small wins.
 Got a “get well soon” card from all my coworkers today, and wow, did that lift my spirits! It was such a thoughtful gesture, and reading everyone’s messages really made me feel supported and connected, even while I’m out of the office. Thanks, team—this was exactly the kind of pick-me-up I needed!
Got a “get well soon” card from all my coworkers today, and wow, did that lift my spirits! It was such a thoughtful gesture, and reading everyone’s messages really made me feel supported and connected, even while I’m out of the office. Thanks, team—this was exactly the kind of pick-me-up I needed!
Today was mostly routine. I kept my foot elevated as much as possible, alternating between stretches and push-ups to stay somewhat active. Spent a good chunk of time researching and browsing online, trying to keep my mind occupied. Foot remains numb. Can’t feel my toes.
The deck was my spot again for reading, weather’s still decent, so I’m trying to enjoy it while I can.
Crutch navigation felt smoother, though the occasional wobble keeps me on edge. Pain was minimal overall, no real discomfort.
22:30 Had my first fall today, coming down two steps with crutches. Wiped out hard and hit the ground before I knew what was happening. I can definitely feel it around my calf now, and there’s this nagging worry that I might’ve messed with the tendon or the sutures. Ugh. I messaged Deanna. She said if bleeding through dressing, go to E.R. otherwise give her an update in the morning.
10/06 Post-Op Day 5
Had a bit of a stumble last night, but luckily no apparent harm done. Slept through the night just fine and woke up feeling good, no lingering pain or soreness from the fall. Took 2 Advil with my morning coffee and keeping the foot elevated as much as possible today. Pain level 1/10. Back to focusing on recovery.
Took another shower today using the Waterproof Leg Cast Cover I got on Amazon. Niki helped get it over the bandaging, and it’s still holding up great. Balanced by keeping my injured foot flat without putting weight on it. Rest of the day was the usual, elevating my foot, staying on top of stretches, and squeezing in some pushups. Routine’s starting to feel more manageable.
10/09 Post-Op Day 8
I’ve been in a steady routine over the last few days, focusing on keeping my foot elevated and managing my time with activities that keep me engaged. Pain has been minimal, hovering around a 1 out of 10, which has made the whole experience much more manageable.
With my appointment with the surgeon coming up on October 10, I’m feeling a mix of anticipation and patience. I’m eager to hear his feedback and discuss the next steps in my recovery process. It’s been a journey of small victories, and I’m ready to embrace whatever comes next.
During this time, I’ve been focusing on light activities, keeping my mind occupied while I rest. The waiting game can be challenging, but I’m trying to stay positive and look forward to the progress ahead.
10/10 Post-Op Day 9
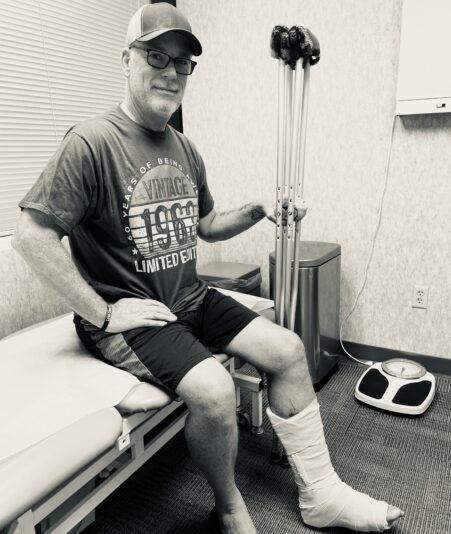
Today was a significant milestone in my recovery journey. I had my follow-up appointment with Dr. Spak, and I walked away with nothing but good news. He removed the stitches, which felt like a small victory in itself. I got fitted for a new, taller boot that comes with a heel wedge for better support. Right out of the box, it includes four wedges total. They took out two of the wedges for me and left the other two in my boot.
The best part? Dr. Spak said I can start putting weight on my foot as comfort allows. No more crutches for me unless I’m covering long distances or not wearing the boot. This feels like a huge step toward regaining my independence. He also mentioned that I don’t have to sleep with the boot on, which is a nice bonus and should make resting a bit more comfortable.
Looking ahead, I’m set to be back at work from home starting Monday, and I’m looking forward to easing back into my routine. Physical therapy should also be starting next week, which I’m excited about. My next follow-up is on October 31, so I’m eager to see how much progress I can make by then. Each day is bringing me closer to recovery, and today just reinforces my optimism. Here’s to the next chapter!
10/12 Post-Op Day 11
The last two days have been great. I’ve officially ditched the crutches around the house, and it’s wild how much of a difference it makes. It’s like I’ve regained a bit of my independence back; simple things like making coffee, getting in the shower, letting the cats in, or just heading to the bathroom have become so much easier.
My calf feels surprisingly good in the boot, and the incision is doing great. I don’t even need to keep my foot elevated as much anymore, maybe only 25% of the time, which is a huge relief. Sleeping without the boot has been a blessing all on its own.
I haven’t felt the need for any meds, not even a Tylenol. My pain level has been at a solid 0/10 for the last two days. It’s been a smooth ride lately, just hoping this trend sticks. Foot remains mostly numb.
10/14 Post-Op Day 13
Today marked my return to working from home. Fortunately, I have the ability to work remotely until I’m ready to return to my hybrid schedule, which will eventually include a few days in the office each week. I spent 10 hours working from my home office, and overall, I felt pretty good throughout the day. I stayed comfortably snug in my boot, and being back in the groove felt reassuring. There’s a sense of normalcy creeping back in, which I definitely welcomed.
10/16 Post-Op Day 15
Today marked a significant milestone in my Achilles recovery. I drove for the first time since surgery. It was just a short trip across town to a doctor’s appointment, but it felt empowering. I parked, navigated with my crutches in and out of the car, and made it back home without issue. It was a small outing, but a real confidence builder as I continue pushing through this recovery phase.
10/17 Post-Op Day 16
 Today was my first physical therapy session, and it feels like a big step forward. My therapist, Rachel, walked me through what to expect in the coming weeks. She checked out my foot and was pretty pleased with how it’s healing, which was great to hear. Rachel gave me four exercises and stretches to work on every day, simple but important moves to keep me progressing. I’ll be seeing her twice a week for the next month, and I’m feeling optimistic about the road ahead. It’s all about slow, steady progress from here.
Today was my first physical therapy session, and it feels like a big step forward. My therapist, Rachel, walked me through what to expect in the coming weeks. She checked out my foot and was pretty pleased with how it’s healing, which was great to hear. Rachel gave me four exercises and stretches to work on every day, simple but important moves to keep me progressing. I’ll be seeing her twice a week for the next month, and I’m feeling optimistic about the road ahead. It’s all about slow, steady progress from here.
10/20 Post-Op Day 19
I’ve been sticking to the rehab exercises that Rachel recommended, doing them at home three times a day. I can definitely feel my lower leg getting stronger. I also removed one of the two remaining heel wedges, so that’s more progress! Plus, I’m still not taking any meds at all.
10/24 Post-Op Day 23
Today’s PT session marked my third, and it was packed with a range of strengthening exercises, including some time on the bike, which felt great to get moving again.

Rachel, my therapist, was pretty upbeat about my progress, she mentioned I’m already showing a lot more flexibility compared to others at this stage, which is encouraging. But she also gave me a word of caution, don’t push it too hard, I need to be patient and let the process play out, even though the temptation is there to go full throttle.
10/26 Post-Op Day 25
Today was a big step forward, literally. I spent the day running errands all over town, moving around without crutches for the first time, just my moon boot supporting me. Even hopped on the John Deere to mulch some leaves and wrapped it up by washing the car. I felt like I could take on anything, as long as I keep a cautious eye on every move. Now, all focus is on Thursday’s checkup with Dr. Spak. Can’t wait to see what he says.
10/31 Post-Op Day 30
Had my one-month follow-up with Dr. Spak, he says my progress is exceptional, and honestly, I felt the same after he answered every single one of my questions with so much patience. I asked about the numbness, and he says it’s still early, give it more time. I’m grateful for his support, and completely trust his judgment, he’s made this process easier.
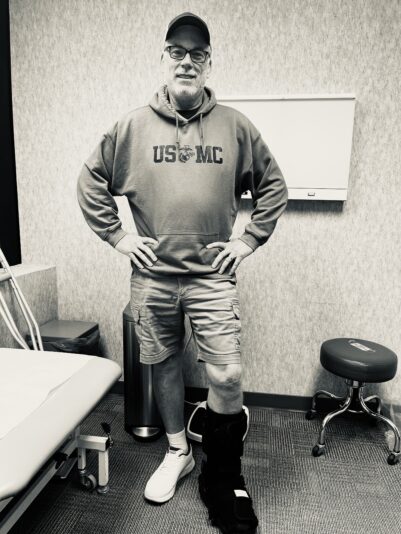
The big news: he’s cleared me for work travel with no restrictions, so I’ve already booked a trip to Sweden for November 17. It’ll be just six weeks post-surgery, and I’ll be back to business. He’s given me the green light to switch back to the shorter boot, minus the heel wedge this time, and I’m officially crutch-free. Physical therapy is now down to once a week, and with no pain in sight, I can also start doing limited walking around the house barefoot. I’m keeping it easy, definitely not looking to push the recovery faster than it should go, but it feels great to be making strides.
11/07 Post-Op Day 37
Returned to the office yesterday for the first time in six weeks, wearing the moon boot and skipping the crutches. Tripled my daily step count and felt the strain by day’s end, but it was the good kind of tired. Awkward with the numbness, like my foot is asleep, which makes me limp. Great to be back in the swing of things and feeling progress.
11/23 Post-Op Day 53
Just got back from a week in Sweden, and it was a solid step forward in my recovery. I wore the moon boot during travel, including at the airports and while boarding and deplaning, but once on the plane, I walked around in socks. Total time in the air was nearly 20 hours. While in Sweden, I worked in the office all day wearing my regular casual shoes. I took it slow, walked with a slight limp, but felt comfortable and not like I was pushing it too hard. Occasionally, my heel would get a little sore, but it wasn’t anything I couldn’t handle. No need for pain meds at all while I was there.
Now that I’m back home and feeling better than ever, I’ve decided I’m pretty much done with the boot. Still have a few weeks of physical therapy left and a follow-up with Dr. Spak coming up soon. Feeling great though!
12/05 Post-Op Day 65
2-Month Post-Surgery Follow-up with Dr. Spak:
Dr. Spak was pleased with my progress but recommended an ultrasound due to swelling around my ankle. The ultrasound confirmed a blood clot (acute, occlusive DVT) in one of the posterior tibial veins in my left leg. The major veins were normal, but the posterior tibial vein is dilated and shows signs of a clot.
Next steps: Dr. King at the vascular clinic put me on Eliquis blood thinner. I’ll have another ultrasound in a few weeks to check how the clot is doing.
01/05 Post-Op Day 96
Had a follow-up ultrasound, and the blood clot has shrunk a bit. Dr. King isn’t overly worried given its size and location, but I’ll stay on the blood thinners for now. Physical therapy continues once a week, and I’m feeling stronger with each session. Swelling is still noticeable, so I’ve been prescribed 20-30 mmHg compression socks to wear, especially when traveling or flying.
01/30 Post-Op Day 121
Had a third ultrasound today to check on the blood clot below my knee. Dr. King isn’t concerned about it due to its location and size. I’ll have another scan in four months, but for now, there are no major issues. I’m still walking with a bit of a limp due to the numbness and as my calf continues to regain strength. No limitations for work or daily activities, but I’m still avoiding sports and running, which will take a few more months.
03/09 Post-Op Day 160
Physical therapy sessions continue, and I’ve been walking a couple of miles a day, stretching, and steadily getting stronger. Still dealing with some tingling in my foot, and my toes feel numb all the time, but overall, things are improving. Progress may be slow, but it’s progress nonetheless.
05/06 Post-Op Day 218
Had a follow-up with Dr. Spak today. I told him the trip to Sweden and India went off without a hitch, no setbacks, no surprises. He was pleased to see the swelling was down compared to my last visit. I did mention that when I walk a mile or more, my foot still feels like it’s on fire and goes numb. Dr. Spak says give it a few more months, he’s optimistic it’ll settle down with time.
08/07 Post-Op Day 311
Saw Dr. Isaac Cohen for nerve testing of the left foot (per Dr. Spak referral) due to persistent paresthesia.
Complaints: Tingling, numbness, and burning in the entire left foot after walking ¼–½ mile; right foot normal.
Physical Exam: Left ankle incision healed; 5/5 strength in lower extremities; reflexes absent in left gastrocsoleus, normal on right. Symptoms partly reproducible with percussion over left superficial peroneal nerve.
Nerve Conduction & EMG:
Left foot sensory nerves (superficial peroneal and sural) absent.
Left tibial motor nerve shows prolonged distal latency and reduced amplitude.
EMG shows moderately increased spontaneous activity in left abductor digiti quinti and diminished recruitment in left abductor hallucis.
Right foot largely normal.
Findings indicate distal sensorimotor neuropathy; age-related changes unlikely.
Clinical Impression: Neuropathy present; not explained solely by Achilles repair, though the injury likely contributed. Recommendation: neurology consult.
Functional Impact: Left foot numb, tingling, painful when walking; cannot walk long distances; right foot fully normal.
Thoughts: Frustrated that testing notes symmetric readings despite right foot being clinically normal. Believe neuropathy is directly caused by Achilles injury. Need neurology evaluation to confirm and strengthen documentation for future treatment and potential claims.
09/19 Post-Op Day 354
Nearly a year after left Achilles rupture, numbness, tingling, and burning in left foot remain relentless. Running is impossible; walking more than a quarter mile triggers severe pain, and even driving can cause flare-ups. Told Deanna today that before the injury, I could walk the high school path near my house easily — now even a short walk feels like my foot is “on fire.”
Called Dr. Spak’s office and Deanna to schedule a neurology appointment for further evaluation. Documenting everything carefully: left foot symptoms are persistent, clearly linked to Achilles injury, and severely limit walking, running, and daily function.
Symptoms and Functional Limitations:
Persistent numbness, tingling, and burning in left foot.
Severe pain after walking more than ¼ mile; running completely impossible.
Pain and paresthesia can occur even during driving.
Foot “feels on fire” after minimal activity.
Left foot weaker and less functional than right foot.
Previously normal activities (walking around high school path) now a struggle.
Significant impact on daily life and mobility.
Reference to 08/07 Nerve Testing:
Left sensory nerves absent; left tibial motor nerve prolonged latency and reduced amplitude.
EMG consistent with distal sensorimotor neuropathy.
Right foot largely normal, despite minor EMG activity.
Dr. Cohen recommended neurology follow-up to further evaluate cause and support treatment/rating documentation.
10/7/2025
Today I saw Dr. Fattahi, neurologist in Middlebury, CT, accompanied by my case worker, Deanna. He confirmed that my left sural nerve is damaged, and the numbness and burning in my foot are likely permanent. He explained that this is a lifetime disability, and that further surgery would not improve the situation. To manage pain, I was prescribed gabapentin. Dr. Fattahi also plans to do his own EMG on 12/16/2025. After the appointment, it really hit me how serious this outcome is and that I need legal representation to make sure my interests are protected moving forward. Functional impact: Walking is still extremely limited, running is impossible, and the burning sensation continues constantly.
NO FURTHER UPDATES, FOR A WHILE
Timeline
09/24 – Injury Day:
Ruptured Achilles playing basketball.
10/01 – Surgery Day:
Achilles repair surgery with Dr. Spak. Crutches and no weight-bearing.
10/04 – 0 months, 0 weeks, 3 days since surgery:
Nerve block wore off. Managed pain with Tylenol and Advil.
10/08 – 0 months, 1 week, 0 days since surgery:
Stitches removed. Upgraded to a taller boot. Limited crutch use.
10/17 – 0 months, 2 weeks, 2 days since surgery:
Started physical therapy twice a week.
10/31 – 1 month, 0 weeks, 2 days since surgery:
One-month check-up. Crutches gone. Smaller boot, no wedge.
11/23 – 1 month, 3 weeks, 2 days since surgery:
Returned from a week in Sweden. Officially done with the boot.
12/05 – 2 months, 0 weeks, 4 days since surgery:
2-month checkup, ultrasound shows I have a blood clot. They put me on Eliquis blood thinner.
01/30 – 4 months, 1 week, 2 days since surgery:
Third ultrasound shows no major concerns. Follow-up scheduled in four months. Still walking with a limp, but improving daily.
03/09 – 5 months, 1 week, 4 days since surgery:
Walking daily, getting stronger. Mild tingling and numbness linger, but the limp is barely there.
04/25 – 6 months, 3 weeks, 3 days since surgery:
Just returned from a 3-week journey across Sweden, India, and back again — zero issues, smooth sailing all the way.
09/19 – 11 months, 2 weeks, 4 days since surgery:
Nearly one-year post-op. Persistent left foot numbness, tingling, and burning; unable to run, walking limited to ~¼ mile before severe pain. EMG and nerve conduction testing by Dr. Cohen show absent sensory responses in left foot and moderate denervation in key foot muscles, confirming neuropathy. Appointment with Dr. Spak on October 6th; actively pursuing neurology consult for further evaluation. Walking uneven, limping, previously normal activities now impossible.
#AchillesSurgery, #AchillesTendonRecovery, #AchillesRupture, #AchillesHealing, #EmbraceTheSuck, #TheSuckLife, #VeteranResilience, #SurgeryRecoveryStory, #RehabJourney, #AchillesTendonSurgery, #AchillesTearRecovery, #PhysicalRehab, #HealingJourney
 Our legacy lives through the stories we tell. The Suck Life wants yours! Make Chesty proud!
Our legacy lives through the stories we tell. The Suck Life wants yours! Make Chesty proud!



 Semper Fidelis
Semper Fidelis



Prayers with you brother! I’m 100% certain Jake is with you during your recovery in his room. My heart almost stopped to read about your fall. Waiting to see if you are not injured by that. Love you. PS using the chair to help you navigate the restroom breaks was a good idea but this is why I suggested the knee scooter. Same idea but easier .