by Wally Beddoe, December 2009
University of Bridgeport, Psychology
Posttraumatic Stress Disorder (PTSD) is a condition that can develop after someone has experienced a life-threatening situation. People with PTSD often can’t stop thinking about what happened to them.  They may try to avoid people and places that remind them of the trauma and may work hard to push thoughts of the event out of their head. Feeling numb is another common reaction. Finally, people find that they have trouble relaxing. They startle easily and are often on guard. (NCPTSD, 2007)
They may try to avoid people and places that remind them of the trauma and may work hard to push thoughts of the event out of their head. Feeling numb is another common reaction. Finally, people find that they have trouble relaxing. They startle easily and are often on guard. (NCPTSD, 2007)
My paper will reflect the symptoms, causes, treatment, and experiences of PTSD as shared by a few Marine friends diagnosed with the disorder; Marines who served one or more tours of duty in combat. Some veterans come out of the battlefield relatively unscathed. Others are so severely traumatized, it takes decades to manage. Earlier generations may have called the condition “Shell Shock”, “Soldier’s Heart”, or “Combat Fatigue”.
Writing a paper about PTSD when one has never experienced it is a tough assignment. I can only imagine the miserable environment of one suffering from this psychological disease.
According to research published in the New England Journal of Medicine, 17% of the troops returning from Iraq and Afghanistan have PTSD. In 1984, the National Vietnam Veterans’ Readjustment Study (NVVRS) found similar rates for Vietnam Veterans. But only about 40% of veterans with PTSD seek treatment. There’s still a stigma attached to PTSD, and veterans with PTSD just can’t get any respect. Post Traumatic Stress Disorder is one of the most debilitating injuries a soldier can suffer in war time. It is life-long condition that can be treated but can never be cured. It’s an ailment that destroys lives.
A 2007 study of combat-exposed Vietnam War veterans shows that those with injuries to certain parts of the brain were less likely to develop PTSD. PTSD involves the persistent reliving of a traumatic experience through nightmares and flashbacks that may seem real. Twenty percent to 30 percent of Vietnam vets (more than 1 million) have been diagnosed with PTSD, and a similar rate has been reported among Hurricane Katrina survivors in New Orleans. Public health officials are currently tracking the disorder among soldiers returning from Iraq. Yet, while war and natural disasters tend to call the greatest attention to PTSD, it’s estimated that millions of Americans suffer from it as a result of assault, rape, child abuse, car accidents, and other traumatic events. (NIH Press, 2007)
BRAIN AND BEHAVIOR
When we study the brain, we learn about the Limbic System, which refers to parts of the brain (forebrain) that are closely associated with fear and response.
The Limbic System has a major role in producing emotion and motivated behavior. The amygdala, in particular, is strongly related to fear. In situations where true danger exists, such as in military combat, the amygdala’s rapid response may aid survival. However, disorder of the brain’s fear system can be very disruptive. An example is the war veteran who involuntarily dives into the bushes when he hears a car backfire. Another important part of the brain and Limbic System is the hippocampus. The hippocampus is important for forming lasting memories and lies inside the temporal lobes, which is why stimulating the temporal lobes can produce memory-like or dream-like experiences. (Coon, & Mitterer, 2007)
As defined in the Diagnostic and Statistical Manual (DSM)-Fourth Edition-Text Revised (DSM-IV-TR), PTSD is an anxiety disorder comprising four major criteria:
1. Exposure to or witnessing an event that is threatening to one’s well-being and responding with intense fear, helplessness, or horror.
2. Symptoms of re experiencing, such as recurrent and intrusive memories, nightmares, a sense of reliving the trauma, or psychological and physiological distress when reminded of aspects of the trauma.
3. Avoidance of thoughts, feelings, or reminders of the trauma, and the inability to recall parts of the trauma, withdrawal, and emotional numbing.
4. Arousal increases, as manifested in sleep disturbance, irritability, difficulty concentrating, hyper vigilance, or exaggerated startle response.
The cause of PTSD is unknown, but psychological, genetic, physical, and social factors are involved. PTSD changes the body’s response to stress. It affects the stress hormones and chemicals that carry information between the nerves (neurotransmitters). Having been exposed to trauma in the past may increase the risk of PTSD. (A.D.A.M., Inc., 2009)
In order to present meaningful information about PTSD, I interviewed some of my good friends; Vietnam Veterans diagnosed with PTSD, and asked them about their experiences.
My first phone call was to a very good friend, Gordon “Bos” Boswell. Bos was a Force Reconnaissance Marine who served 23 months in Vietnam. He was shot on three separate occasions and medically evacuated by helicopter each time. Once, while in a very bad place called the Bo Bans, walking point with his best friend Christopher Six, Christoper stepped on a ‘Bouncing Betty’ mine. When triggered, these mines launch into the air and then detonate at about waist height. The explosion projects a lethal shower of steel balls and steel fragments in all directions. No words can describe the scene. Bos was yelling at his friend “Don’t die on me!” but there was nothing he could do. Christopher died in Bos’ arms. He then applied a tourniquet on another friend who lost his arm in the same explosion. “At this point, I completely lost it” said Bos. Four Marines died. Bos and two others were also shot or wounded. Continuous exposure to this type of environment challenges a human’s psychological tolerance.
When Bos was discharged from the Marines in 1971, he said he had no emotions [left] whatsoever. He was numb, like a rock. He attended LSU where there was protesting going on. He was embarrassed to tell anyone that he was a Vietnam Veteran. Even his girlfriend and future wife Cheryl did not know. The years following Vietnam were very hard for Bos. He suffered from rage, screaming nightmares of never-ending fights, and sweating terribly. “The slightest thing would just set me off” explained Bos. There were countless scuffles and fist fights. For six years he went to a mental health counselor. “He was no good and he had no clue” Bos told me.
Around 1995, Bos received some direction from friend and fellow veteran Michael Rodriguez.  Michael suggested that either he ends up in a vet hospital or he gets help in an outpatient clinic that he could recommend. Bos followed the advice of his good friend and went to the outpatient clinic where he met Dr. Simpson. Bos was tested for PTSD and in 1996 was diagnosed with 70% disability due to PTSD and Agent Orange. Bos says he was shocked when Dr. Simpson told him “I hate to tell you, PTSD is a progressive disease, it doesn’t get better and there’s no cure for it”. Dr. Simpson treated the PTSD by prescribing Xanax, a medicine used to treat anxiety and panic disorder. “It definitely helps, makes me much more laid back” said Bos.
Michael suggested that either he ends up in a vet hospital or he gets help in an outpatient clinic that he could recommend. Bos followed the advice of his good friend and went to the outpatient clinic where he met Dr. Simpson. Bos was tested for PTSD and in 1996 was diagnosed with 70% disability due to PTSD and Agent Orange. Bos says he was shocked when Dr. Simpson told him “I hate to tell you, PTSD is a progressive disease, it doesn’t get better and there’s no cure for it”. Dr. Simpson treated the PTSD by prescribing Xanax, a medicine used to treat anxiety and panic disorder. “It definitely helps, makes me much more laid back” said Bos.
Bos wrapped up my interview by reiterating “PTSD is the real deal.” He added, “My wife has PTSD from putting up with my [antics] for the first 15 years of our marriage. She’s a good woman! These days I keep a level head, stay away from bad places because I can snap in a heartbeat. I take my Xanax with the morning cup of coffee and it definitely helps.” (G. Boswell, personal communication, November 20, 2009)
On Bos’ personal website, he writes “Sometimes, I awake in the middle of the night, drenched in sweat, and I know I’ve been walking through the Bo Bans again; the place continues to haunt me. I wonder if some present-day Vietnamese ever sees the ghost of the young man I once was, wandering through the Bo Bans”.
In response to a PTSD posting on a veteran website I maintain, a few friends responded:
“Hi Wally, I was diagnosed with PTSD about 5 years ago. I didn’t know what it was all about and didn’t know I had it until I was asked some very emotional questions from a shrink at the VA. The biggest obstacle is admitting to yourself that you have PTSD. Once you understand what its’ all about you can start to manage the symptoms. There is no cure but you can function. I wear rubber band on my wrist and whenever PTSD interrupts rational thinking I snap the band. Most times that is all you need to break the thought pattern. The VA tries to drug you up but it doesn’t work for me. Only makes it worse. NO DRUGS FOR ME. PTSD not only affects the person but everyone that is close to you. I wonder how my wife and family were able to put up with me all those years.”
(Jardo Opocensky, personal communication, November 9, 2009)
“Wally, you will get lots of opinions but no answers except an acknowledgment that it exists in some form. I have one axe to grind: For compensation, the VA seems to seek one incident. Hell, we all can probably site 365 or more! That is my issue in a nutshell. Imagine driving the roads daily in Iraq and then coming home to drive on our highways, hit by an IED or not. PTSD? You betcha! I submit that constant stress, especially under threat of death or injury, can cause problems even more than just one incident. You have a secondary problem in that if the VA is going to pay for PTSD then everyone will put in for it, real, imagined, or fake. Let me share a personal experience. Last May, while out for a run, I was hit from the rear by a bicyclist. The fall broke my right shoulder and my arm. After six months of rehab I am back to running. Now, if anyone comes up behind me while running, I jump in fear. Am I suffering from PTSD or am I reacting as any normal person would? So, it is an issue that merits your study. Thank you. SF, /s/ Ray.”
(Raymond J. Norton, personal communication, November 9, 2009)
“Good luck Wally, I don’t know that the VA really understands it! The shrink I see at the VA has commented that the condition seems to be surfacing at a faster rate now among Vietnam vets than in the past. His theory is that the majority of us came back, threw ourselves into whatever we did the rest of our lives and functioned well as long as we stayed busy and were working ourselves to a point of exhaustion. Now that we are starting to slow down, more of us have problems. Mine is a mild case manifested by bouts of depression. Of course, many of my old Corps friends thought I was crazy anyway, so it might be hard to tell the difference.”
(Bob Quinter, personal communication, November 9, 2009)
“Wally, I was diagnosed in the 70s and went to some VA outreach programs that showed me that there were a lot of really messed up people that made me feel like I was OK… Realized that half the battle has just understanding why I felt and behaved the way I did, I wanted to be away from people especially crowds; did not want to stay in one place too long; felt like I was tuned in to a different world than most other people. After flying as a Gunner on the Huey gunships, it is very hard to go back to the States and be able to replicate the adrenaline rushes. Closest you can come is Police work which I did for four years. Alcohol allowed me to get to sleep at night. Once I had some spare time on my hands the PTSD started to get me freaky and so I went to the VA and after 2 years of meds and meetings my wife told me I’m almost able to get along well with others. Two weeks ago I started bleeding internally and when I went to the VA my doctor said the Citalopran that I was taking could in some cases cause life threatening internal bleeding and she took me off all my meds pending the results of an upcoming colostomy; Back to the beer. Semper Fi, Phillip D. Moss, VMO-2, 1968-1970.”
(Phillip D. Moss, personal communication, November 9, 2009)
A publication by the Psychopharmacology Unit, University of Bristol, United Kingdom, reflects best what I found repeatedly in my interaction with my veteran friends, which are the parts of the brain affected by PTSD.
The publication states “PTSD is a highly disabling condition that is associated with intrusive recollections of a traumatic event, hyperarousal, avoidance of clues associated with the trauma, and psychological numbing. The field of neuroimaging has made tremendous advances in the past decade and has contributed greatly to our understanding of the physiology of fear and the pathophysiology of PTSD. There appear to be 3 areas of the brain that are different in patients with PTSD compared with those in control subjects: the hippocampus, the amygdala, and the medial frontal cortex. The amygdala appears to be hyper reactive to trauma-related stimuli. The hallmark symptoms of PTSD, including exaggerated startle response and flashbacks, may be related to a failure of higher brain regions (i.e., the hippocampus and the medial frontal cortex) to dampen the exaggerated symptoms of arousal and distress that are mediated through the amygdala in response to reminders of the traumatic event.” Further, the analysis read in addition to the high rate of PTSD exposure to combat exposure, risk for PTSD is also higher when a physical injury has been received. For example, two to three times higher rates of PTSD have been found among injured Vietnam veterans compared with non-injured veterans. (JRRD, 2007)
Kolb (1987) proposed a neuropsychological explanation of intrusive memories and associated psychophysiological arousal in PTSD. He has supplemented a two-factor learning theory that PTSD results from both classical conditioning of extreme emotional responses to traumatic stimuli (i.e., fear, terror, anger, rage, sadness, guilt, and indignation) and operant conditioning of emotional numbing, withdrawal, and avoidance of traumatic stimuli (Kolb, 1987). He proposed that PTSD results from excessive traumatic stimulation that overwhelms the capacity to process information efficiently. Such stimulus overload occurs when the … capacity to process information signaling threat to life overwhelms the cortical … processes concerned with perceptual discrimination and effective adaptive responses for survival (Kolb, 1987).
TREATMENT: USING PRINCIPLES TO SOLVE THE PROBLEM
Cognitive Behavior Therapy – Exposure to memories and reminders of the original trauma
-In the 1980’s, Dr. Terence M. Keane and his colleagues found that exposure therapy was effective in treating the PTSD symptoms of Vietnam War veterans. Exposure therapy, previously known as imaginal flooding therapy, involves carefully exposing the patient to prolonged and repeated imagined images of the trauma until the images no longer cause severe anxiety. In Keane’s randomized clinical trial involving 24 Vietnam veterans, Keane found that exposure therapy was effective in reducing many of the veteran’s PTSD symptoms, including nightmares, flashbacks, memory and concentration problems, and irritability.
Other treatments include:
Eye Movement and Desensitization Reprocessing (EMDR), which is very controversial.
Critical Incidents Stress Debriefing (CISD), which is immediate treatment of trauma; and also very controversial.
Exposure; Facing the situation or object that triggers anxiety (memory and cue dependency).
In flooding, feared stimuli are presented to the patient at full intensity, not gradually.
Medications such as Anxiolytics and drugs that reduce anxiety like Valium and Xanax
Antidepressants (Tricyclics and Selective Serotonin Reuptake Inhibitors (SSRIs)
SUMMARY
My research indicates that while there may not be a solution to PTSD, approaches to controlling the effects of PTSD include communication, education, research & development, medical, and therapeutic efforts. Most important is that veterans or PTSD sufferers communicate with others if they feel they may have PTSD. Understanding PTSD and knowing what the options are for treating it is very important. Active-duty troops must be educated and made aware of PTSD and can recognize the signs in themselves or their comrades. Continued research and development is vital to learning more about the brain and how it processes fear and stress. Medical research and drug testing must continue. Research available therapy opportunities for dealing with PTSD are also critical. Dr. Keane suggests cognitive behavioral therapy can be used to access emotions associated with the traumatic event and promote emotional processing. It is this emotional processing that is viewed by many experts as the essential ingredient for treating PTSD.
I’m grateful to my Marine Brothers who supplied information pertaining to their PTSD. I believe communication is a large part of the dealing and healing process. The more we know about PTSD, the more we can help those who suffer from the symptoms that cripple lives of veterans and their families, co-workers, and friends.
Work Cited:
Coon, D, & Mitterer, J. (2007). Introduction to psychology. Belmont, CA: Thomson Higher Education.
NCPTSD. (2007, May 22). P common reactions after trauma. Retrieved from https://ncptsd.va.gov/ncmain/ncdocs/fact_shts/fs_commonreactions.html
JRRD. (2007). Posttraumatic stress disorder and posttraumatic stress disorder-like symptoms and mild traumatic brain injury. Retrieved from https://www.rehab.research.va.gov/jour/07/44/7/kennedy.html
Kolb, L. (1987). A neuropsychological hypothesis explaining posttraumatic stress disorder. American Journal of Psychiatry, 144: 989-995.
A.D.A.M., Inc. (2009). Post-traumatic stress disorder. Retrieved from https://health.google.com/health/ref/Post-traumatic+stress+disorder
NIH Press. (2007, December 26). Study suggests some brain injuries reduce the likelihood of post-traumatic stress disorder . Retrieved from https://www.gluvsnap.com/news/New_Online_Features_Translate_Vision_Science_to_Everyday_Life%20_51.html
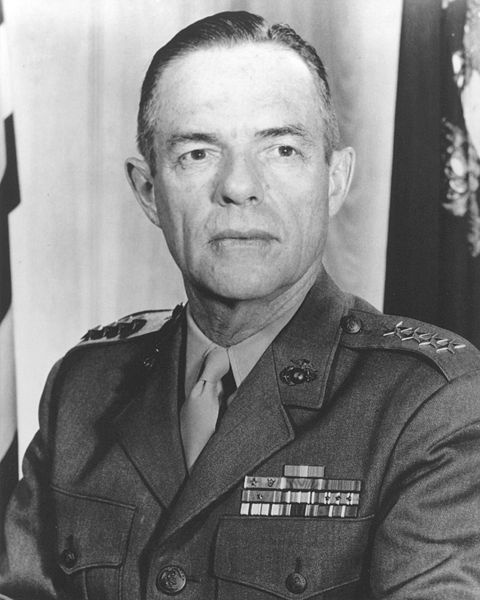
 Our legacy lives through the stories we tell. The Suck Life wants yours! Make Chesty proud!
Our legacy lives through the stories we tell. The Suck Life wants yours! Make Chesty proud!



 Semper Fidelis
Semper Fidelis


BEEN READING YOUR BOOK REPORTS & PAPERS
FOR THE LAST 2 PLUS HOURS ITS 4:10 AM
ISN’T PTSD WONDERFUL
I FLEW WITH HMM-363 IN 66/67/68
I NOW HAVE A LOT OF NEW BOOKS TO READ
I MET YOU THROUGH BUZZ SHANTY IN DC
HAVE NO IDEA HOW I GOT TO YOUR PAGE WAS
ON POPASMOKE LOOKING FOR OBIT FOR STEVE
BACKLUND BUZZ’S BROTHER INLAW DIED 10/2/12
ALSO A HMM-363 BROTHER
THANK YOU FOR HELPING ME THROUGH THE NIGHT
SEMPR FI
>Hypnosis can also help in recovering traumatic experiences. Learning to survive the experience will make us better and healthier human beings.